Utilization of carbetocin for prevention of postpartum hemorrhage after cesarean section: a randomized clinical trial
Franco Borruto · Alain Treisser · Ciro Comparetto
Abstract
Purpose A randomized study involving pregnant women was conducted to compare the eVectiveness of a single intravenous (IV) injection of carbetocin with that of a stan- dard 2-h oxytocin IV infusion with respect to intraoperative blood loss in the prevention of uterine atony after cesarean section (CS). The two treatments also were compared for safety and ability to maintain adequate uterine tone and to reduce the incidence and severity of postpartum hemor- rhage (PPH) in women at risk for this condition.
Methods Between 1 September 2007 and 5 January 2008, we enrolled 104 patients with at least one risk factor for PPH undergoing CS in a randomized, controlled clinical trial. We compared the eVect of a single 100 microg IV dose of carbetocin with that of a standard 2-h ten interna- tional units (IU) IV infusion of oxytocin. The primary out- come was the proportion of patients requiring additional oxytocic intervention for uterine atony. Fiftytwo women received 100 microg carbetocin IV immediately after placental delivery, while 52 women received 10 IU oxyto- cin IV infusion. Complete blood count was collected at entry and 24 h postpartum. All outcome measures, includ- ing the need for additional uterotonic agents or uterine mas- sage, and blood loss, were analyzed using chi-square, Fisher exact, and Student’ s t tests.
Results A single 100 microg IV injection of carbetocin was as eVective as a continuous 2-h infusion of oxytocin in controlling intraoperative blood loss after placental delivery. Mean blood loss after carbetocin administration was 30 ml less than after oxytocin administration (P = 0.5). The percentage of patients with blood loss ·500 ml was greater with carbetocin (81 vs. 55%; P = 0.05). Carbetocin enhanced early postpartum uterine involution. The fundus was below the umbilicus in more patients who received car- betocin at 0, 2, 6, and 24h on the ward (P<0.05). The main additional uterotonic agent used was a further admin- istration of oxytocin (20IU in physiological solution 500 ml at an infusion rate of 200 ml/h). In the carbetocin group, 20 of the 52 women (38.4%) required at least one uterine massage compared to 30 of the 52 women (57.7%) in the oxytocin group (P < 0.01). Overall, uterotonic inter- vention was clinically indicated in two of the women (3.8%) receiving carbetocin compared to Wve of the women (9.6%) given an IV oxytocin infusion (P < 0.01). The odds ratio of treatment failure requiring oxytocic intervention was 1.83 (95% conWdence interval, CI, 0.9–2.6) times higher in the oxytocin group compared with the carbetocin group.
Conclusions Carbetocin makes possible to obtain, with a single IV injection, results equivalent to those of oxytocin on the maintenance of uterine tonicity and the limitation of blood losses, in the peri- and in the post-operative period, during a delivery by CS. It has in addition a comparable tol- erance. Even in our series adverse events are practically of the same type and similar frequency in both study groups. Thus, the eVectiveness of carbetocin consists, thanks to its long half-life, on an unique injection, whereas oxytocin requires repeated injections or a perfusion of several hours, with a variability of the administered doses.
Keywords Postpartum hemorrhage · Carbetocin · Cesarean section · Oxytocin · Third stage of labor
Introduction
Despite evidence that active management of the third stage of labor reduces the incidence of PPH, deWned as blood loss ̧ 500 ml and/or the need for a blood transfusion within 24h of delivery, expectant management is still widely practised. Factors accounting for this situation include the desire for a more natural experience of child- birth, the philosophy that active management is unneces- sary in low-risk women, and avoidance of the adverse eVects of conventional uterotonic agents [2, 3].
Uterine atony is the Wrst cause of hemorrhages at the time of delivery. Together with its prevention, its treatment is to be considered within a context of public health. Post- partum hemorrhage in cases of delivery programmed by cesarean section (CS), has a quite real gravity. It is indeed one of the main causes of maternal mortality. Thus, the need for decreasing the rate of PPH is today a concern for all the obstetric units.
To face it, the mean tools on which we count are the improvement of monitoring, the deWnition of strategies based on standardized protocols, and a prophylactic treat- ment having an eVective constrictive action on the uterus.
A long-acting oxytocin analog, 1-deamino-1-monoc- arba-(2-O-methyltyrosine)-oxytocin [d(COMOT)], car- betocin (Fig. 1), is indicated in the prevention of uterine atony following a delivery by CS, under peridural or rachianesthesia.
A randomized study involving pregnant women was conducted to compare the eVectiveness of a single intrave- nous (IV) injection of carbetocin with that of a standard 2-h oxytocin IV infusion with respect to intraoperative blood loss in the prevention of uterine atony after CS. The two treatments also were compared for safety and ability to maintain adequate uterine tone and to reduce the incidence and severity of PPH in women at risk for this condition.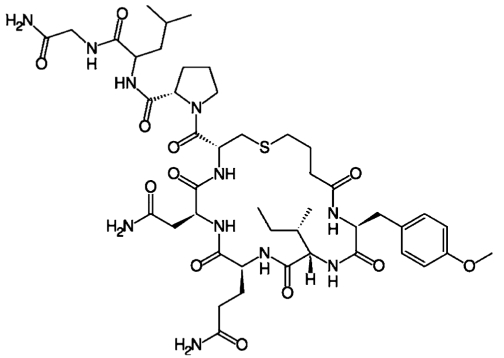
Fig. 1 Chemical formula of carbetocin
Materials and methods
Between 1 September 2007 and 5 January 2008, we enrolled 104 patients with at least one risk factor for PPH undergoing CS in a prospective, randomized, controlled clinical trial. The patients were divided in two groups with blinding to the study medication.
We compared the eVect of a single 100 microg IV dose of carbetocin with that of a standard 2-h ten international units (IU) IV infusion of oxytocin. The primary outcome was the proportion of patients requiring additional oxytocic intervention for uterine atony. A variable sample size, sequential design was used.
There was not much diVerence in the demographic vari- ables between the two groups. Only term pregnancies (after 36 weeks) with singleton fetuses were included. Toxemia, eclampsia, and epilepsy were considered contraindications to the treatment.
The main predictors for PPH were (Table 1): co-existing hypertension (26 cases, 25%), chronic anemia (18, 17.3%), low socio-economic background (16, 15.4%), past history of PPH (12, 11.5%), previous delivery by CS (10, 9.6%),
Table 1 Risk factors for PPH
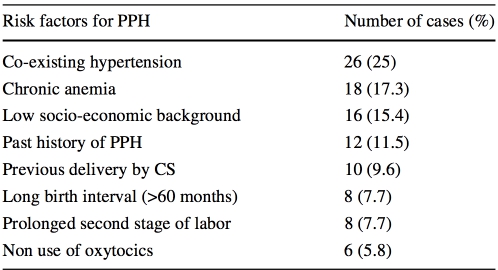
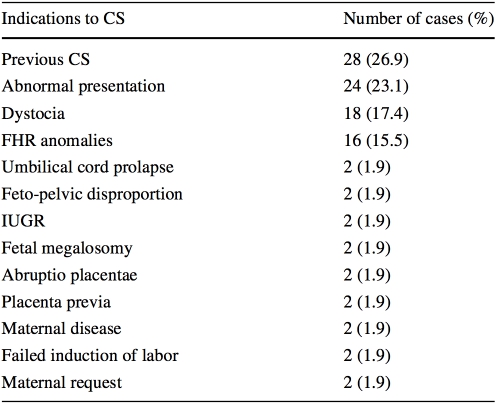
Table 2 Indications to CS
long birth interval of more than 60 months (8, 7.7%), pro- longed second stage of labor (8, 7.7%), and non use of oxytocics (6, 5.8%).
Cesarean section were a mixture of planned and emer- gency interventions, and were performed for the following reasons (Table 2), including history of previous CS (28 patients, 26.9%), abnormal presentations (above all breech) (24, 23.1%), dystocia (18, 17.4%), fetal heart rate (FHR) anomalies (16, 15.5%), and other conditions, such as umbilical cord prolapse, feto-pelvic disproportion, intra- uterine growth retardation (IUGR), fetal megalosomy, abruptio placentae, placenta previa, maternal diseases (such as severe ophtalmopathy), failed induction of labor, and maternal request (two cases, 1.9%, for each one).
The study drug was administered by IV injection to the women during CS after removal of the placenta; blood was collected until abdominal closure. Intraoperative blood loss was calculated with a sensitive colorimetric method. Posi- tion, tone of the fundus, and vital signs were assessed up to 24 h after the operation. The need for additional uterotonic agents was recorded.
Fifty-two women received 100 microg carbetocin IV immediately after placental delivery, while 52 women received 10 IU oxytocin IV infusion. Complete blood count was collected at entry and 24 h postpartum. All outcome measures, including the need for additional uterotonic agents or uterine massage, and blood loss, were analyzed using chi-square, Fisher exact, and Student’s t tests. SigniW- cance was considered for a value of P < 0.05.
All patients were enrolled for the study after informed consent. The study was approved by the Internal Ethical Committee of the Hospital and has been carried out in accordance with the Code of Ethics of the Declaration of Helsinki.
Results
Mean gestational age was 39.1 weeks. The age of the patients ranged between 22 and 41 years. The mean age was 32.2years. As regards to parity, in 71.1% of the patients it was 0000 or 1001.
The mean incision to delivery interval, operating time, and blood loss were 3, 28 min, and 600 ml, respectively.
IV injection of 100 microg of carbetocin produced a tetanic uterine contraction within 3min, lasting about 5 min, followed by rhythmic contractions for a further 50 § 20 min. Adverse eVects of the treatment were not sig- niWcantly diVerent between the two drugs. Both of them, in fact, produced decrease in blood pressure, nausea and vom- iting, Carbetocin produced mild lower abdominal cramping in 21 patients (40.3%) and severe pain in 1 patient (1.9%). These latter symptoms were referred particularly after ces- sation of the eVect of peridural anesthesia. Approximately half of the patients in the two study groups also experienced Xushing and warmth (Table 3).
A single 100 microg IV injection of carbetocin was as eVective as a continuous 2-h infusion of oxytocin in control- ling intraoperative blood loss after placental delivery. Mean blood loss after carbetocin administration was 30 ml less than after oxytocin administration (P = 0.5). The percentage of patients with blood loss · 500 ml was greater with car- betocin (81 vs. 55%; P = 0.05). Carbetocin enhanced early postpartum uterine involution. The fundus was below the umbilicus in more patients who received carbetocin at 0, 2, 6, and 24 h on the ward (P < 0.05). There were no signiW- cant diVerences in uterine tone or type or amount of lochia. Vital signs and hematologic values were comparable in each group, conWrming similar safety proWles.
Population proWle and risk factors for PPH were similar for each group. However, in the carbetocin group, 20 of the 52 women (38.4%) required at least one uterine massage compared to 30 of the 52 women (57.7%) in the oxytocin group (P < 0.01). Mean time from study drug to Wrst mas- sage was 50 min (no signiWcant diVerence between the two drugs).
The main additional uterotonic agent used was a further administration of oxytocin (20 IU in physiological solution 500 ml at an infusion rate of 200 ml/h). Additional oxyto- cin was used to treat seven patients (6.7%) for PPH or per- sistent uterine atony. Overall, uterotonic intervention was clinically indicated in two of the women (3.8%) receiving carbetocin compared to Wve of the women (9.6%) given an IV oxytocin infusion (P < 0.01) (Fig. 2; Table 4). Mean time from study drug to additional uterotonic medication was 60 min (no signiWcant diVerence between the two drugs). There were no diVerences in laboratory PPH indica- tors between the two groups.
Table 3 Side eVects of carbetocin and oxytocin
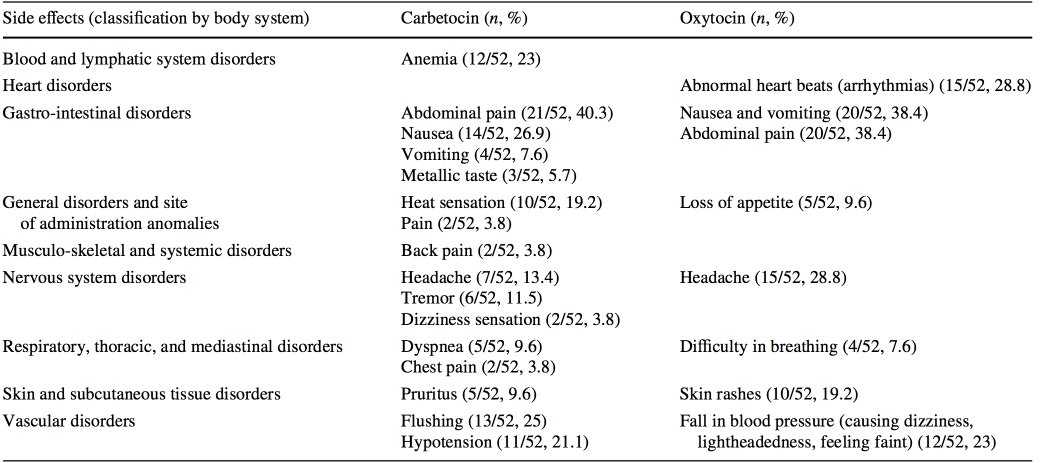
Fig. 2 Proportion of patients requiring uterine massage and utero- tonic intervention
The odds ratio (OR) of treatment failure requiring oxyto- cic intervention was 1.83 (95% conWdence interval, CI, 0.9–2.6) times higher in the oxytocin group compared with the carbetocin group.
Discussion
Postpartum hemorrhage is one of the major contributors to maternal mortality and morbidity worldwide. Active man- agement of the third stage of labor has been proven to be eVective in the prevention of PPH [4–6].
Since publication of the Wrst systematic review compar- ing active with expectant management in 1988 [7], active management of the third stage using oxytocics has become
Table 4 Comparison of results between the two study drugs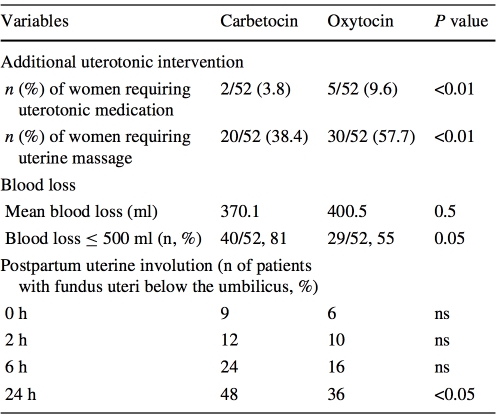
increasingly adopted. Recent surveys, however, show that there are still wide variations in practice around the world [2].
Casuistics of zoo animals with dystocia (Anoa, GiraVe, Snow goat, Scimitar horned Antelope, Bactrian camel, Tiger, Diana monkey) treated with special pharmaceuticals (glucocorticoids, cienbuterol, denaverine, carbetocin) and distance injections by blow darts have been presented. These procedures are described as very eVective and safe methods of obstetrics in zoo animals [8–15].
To determine if the use of oxytocin agonist is as eVective as conventional uterotonic agents for the prevention of PPH, and assess the best routes of administration and optimal doses of oxytocin agonist, randomized controlled trials were reviewed by Su et al. [6]. Four studies (1,037 women) were included in this metanalysis (3 studies on CS and 1 on vagi- nal delivery). Carbetocin is associated with a reduced need for uterine massage in both CS and vaginal deliveries (RR 0.38, 95% CI 0.18–0.80; RR 0.70, 95% CI 0.51–0.94), respectively. However, this outcome measure was only docu- mented in one study on CS and in the only study on vaginal delivery. Pooled data from the trials did not reveal any statis- tically signiWcant diVerences in terms of the adverse eVects between carbetocin and oxytocin. According to this review, there is insuYcient evidence that 100 microg of IV carbeto- cin is as eVective as oxytocin to prevent PPH. In comparison to oxytocin, carbetocin was associated with reduced need for additional uterotonic agents, and uterine massage. There was limited comparative evidence on adverse events.
Uterotonic drugs have been widely used to prevent and to treat PPH. Syntometrine is an eVective uterotonic agent used in preventing primary PPH but has adverse eVects including nausea, vomiting, hypertension, and coronary artery spasm. Leung et al. compared the eYcacy and safety of intramuscular (IM) carbetocin with IM syntometrine in preventing primary PPH in a prospective, double-blinded, randomized controlled trial conducted in a delivery suite of a university-based obstetrics unit on women with singleton pregnancy achieving vaginal delivery after and throughout 34 weeks. Intramuscular carbetocin was as eVective as IM syntometrine in preventing primary PPH after vaginal delivery. It was less likely to induce hypertension and had a low incidence of adverse eVect. So, it should be considered as a good alternative to conventional uterotonic agents used in managing the third stage of labor [6, 16].
Carbetocin appears to be more eVective than a continu- ous infusion of oxytocin and has a similar safety proWle [17]. A single 100 microg IV injection of carbetocin is as eVective and more reliable than a standard continuous infu- sion of oxytocin in maintaining adequate uterine tone and preventing excessive intraoperative blood loss during CS after delivery of the placenta. It makes possible to prevent excessive bleedings, which are increased in cases of insuY- cient uterine tonicity. Its activity begins quickly with valid contractions obtained in 2–3 min. Patients receiving car- betocin require less intervention. It is well tolerated [5] and it has a longer time of action (approximately 5 h) than oxy- tocin (1 h and 30 min).
We classically call “forth stage of labor” the Wrst 24 h which follow delivery; this period is crucial, because at high-risk for hemorrhages. In the peri-operative period, it is easy to check uterine tonicity manually, and also by the visual appreciation of blood losses. In this regard, follow- ing the results of the ConWdential Enquiries into Maternal Deaths report, which claims two maternal deaths annually in the United Kingdom (UK) from PPH, the accuracy of “visual estimation of blood loss” was assessed and suitable pictorial and written algorithms were produced to aid in the recognition and management of massive obstetric hemor- rhage in an observational study to determine discrepancy between actual blood loss (ABL) and estimated blood loss (EBL) conducted by Bose et al., who concluded that accu- rate visual estimation of blood loss is known to facilitate timely resuscitation, minimising the risk of disseminated intravascular coagulation (DIC) and reducing the severity of hemorrhagic shock. Participation in clinical reconstruc- tions may encourage early diagnosis and promptv treatment of PPH. Written and pictorial guidelines may help all staV working in labor wards [18].
Of course, blood loss must be related to the type of patients; 500 ml can be nothing in a “normal” patient but perhaps are “many” in a patient with chronic anemia. A deWnition that today is taking place is: “any blood loss that would result in signs and symptoms of hemodynamic insta- bility or bleeding that induce hemodynamic instability if not properly treated”.
The quality of uterine contractions was considered to be good after the administration of carbetocin, as we could check it in our study on the eVects of carbetocin versus oxy- tocin in patients for whom a CS was performed. This popu- lation was homogeneous in terms of anesthesia and hemodynamic stability, which allowed a comparison of the two molecules.
One of the criteria deWned in this study to evaluate the eVectiveness of carbetocin compared to oxytocin (molecule of reference) was uterine height under the umbilical point after the administration of the drug (carbetocin or oxyto- cin). Thus, it was shown that the percentage of patients hav- ing a uterine height under the umbilical point after administration of the drug was signiWcantly more important in the carbetocin group than in the oxytocin group. This result is a good clinical prove of the eVectiveness of car- betocin on uterine tonicity.
Carbetocin is well tolerated and the monitoring up to 24 h after the administration shows a great hemodynamic stability, comparable with that of oxytocin. Adverse eVects were similar for frequency and nature to those observed with oxytocin. weats can be a little more frequent than with oxytocin; it is a known eVect, due to the surge of blood in general circulation during delivery. There can exist abdom- inal pains like cramps due to uterine contractility, but for the clinician, it is rather the sign that the drug is eVective on uterine tonicity and that the required objective is achieved.
To our knowledge, there are not speciWc studies of the interactions carried out with carbetocin. Nevertheless, we did not observe any pharmacological interaction with the drugs used in the peri-operative period by the anesthetists or with the drugs used in the postpartum period.
Before the availability of carbetocin, the practice in terms of monitoring and management of the patients varied among the teams and the countries. The duration and the dose of an oxytocin perfusion as well as the post-operative monitoring were not homogeneous. The use of carbetocin allowed a certain homogenisation of the practice. From now on, it is enough to make an injection of carbetocin in the operating room; the post-operative follow-up is then simpliWed [19].
Conclusion
Carbetocin makes possible to obtain, with a single IV injec- tion, results equivalent to those of oxytocin on the mainte- nance of uterine tonicity and the limitation of blood losses, in the peri- and in the post-operative period, during a deliv- ery by CS. It has in addition a comparable tolerance. Even in our series adverse events are practically of the same type and similar frequency in both study groups.
Thus, the eVectiveness of carbetocin consists, thanks to its long half-life, on an unique injection, whereas oxytocin requires repeated injections or a perfusion of several hours, with a variability of the administered doses [5].
By its long duration of action and its simpleness of use, carbetocin makes possibile the standardization of proce- dures, unanimously felt today as indispensable. It favour- ishes the production of simple, reproducible, and applicable protocols in all centers, in order to improve the prevention of uterine atony and its complications.
Lastly, carbetocin is currently the subject of studies for new indications: for example, it requires further evaluation particularly for use after vaginal births [2]. But as for today, carbetocin works well in the preventive strategy, and the current experience is suYcient to aYrm that carbetocin is an interesting therapeutic alternative to oxytocin in the prevention of uterine atony after delivery by CS.
Conflict of interest statement Authors do not have a Wnancial rela- tionship with the organization that sponsored the research. They also state that they have had full control of all primary data and that they agree to allow the Journal to review their data if requested.
References
-
McDonald S (2007) Management of the third stage of labor. J Midwifery W omens Health 52:254–261. doi:10.1016/j.jmwh. 2007.02.012
-
Chong YS, Su LL, Arulkumaran S (2004) Current strategies for the prevention of postpartum haemorrhage in the third stage of labour. Curr Opin Obstet Gynecol 16:143–150. doi:10.1097/ 00001703-200404000-00008
-
Mousa HA, Cording V, AlWrevic Z (2008) Risk factors and inter- ventions associated with major primary postpartum hemorrhage unresponsive to Wrst-line conventional therapy. Acta Obstet Gyne- col Scand 87:652–661. doi:10.1080/00016340802087660
-
Wandabwa J, Doyle P, Todd J et al (2008) Risk factors for severe post partum haemorrhage in Mulago hospital, Kampala, Uganda. East Afr Med J 85:64–71
-
Hunter DJ, Schulz P, Wassenaar W (1992) EVect of carbetocin, a long-acting oxytocin analog on the postpartum uterus. Clin Phar- macol Ther 52:60–67
-
Su LL, Chong YS, Samuel M (2007) Oxytocin agonists for pre- venting postpartum haemorrhage. Cochrane Database Syst Rev 3:CD005457
-
Prendiville WJ, Harding JE, Elbourne DR et al (1988) The Bristol third stage trial: active versus physiological management of third stage of labour. BMJ 297:1295–1300
-
Eulenberger K (2000) Medical treatment of dystocia in zoo ani- mals. Dtsch Tierarztl Wochenschr 107:512–515
-
Handler J, HoVmann D, Weber F et al (2006) Oxytocin does not contribute to the eVects of cervical dilation on progesterone secre- tion and embryonic development in mares. Theriogenology 66:1397–1404. doi:10.1016/j.theriogenology.2006.04.032
-
Cort N, Einarsson S, Aström G (1982) EVect of oxytocin and its long-acting analog on milk let-down and intramammary pressure in healthy lactating sows. Am J Vet Res 43:1283–1285
-
Atke A, Vilhardt H (1987) Uterotonic activity and myometrial receptor aYnity of 1-deamino-1-carba-2-tyrosine(O-methyl)-oxy- tocin. Acta Endocrinol (Copenh) 115:155–160
-
Dansereau J, Joshi AK, Helewa ME et al (1999) Double-blind comparison of carbetocin versus oxytocin in prevention of uterine atony after cesarean section. Am J Obstet Gynecol 180:670–676. doi:10.1016/S0002-9378(99)70271-1
-
Norström A, Andersson A, Vilhardt H (1990) Contractile eVect of oxytocin and 1-deamino-1-carba-2-tyrosine (O-methyl)-oxytocin in myometrial tissue from non-pregnant and term pregnant wom- en. Acta Endocrinol (Copenh) 122:566–568
-
Engstrøm T, Barth T, Melin P et al (1998) Oxytocin receptor binding and uterotonic activity of carbetocin and its metabolites following enzymatic degradation. Eur J Pharmacol 355:203–210. doi:10.1016/S0014-2999(98)00513-5
-
Boucher M, Horbay GL, GriYn P et al (1998) Double-blind, ran- domized comparison of the eVect of carbetocin and oxytocin on intraoperative blood loss and uterine tone of patients undergoing cesarean section. J Perinatol 18:202–207
-
Bajcsy AC, Szenci O, van der Weijden GC et al (2006) The eVect of a single oxytocin or carbetocin treatment on uterine contractility in early postpartum dairy cows. Theriogenology 65:400–414. doi:10.1016/j.theriogenology.2005.05.040
-
Silcox J, Schulz P, Horbay GL et al (1993) Transfer of carbetocin into human breast milk. Obstet Gynecol 82:456–459
-
Leung SW, Ng PS, Wong WY et al (2006) A randomised trial of carbetocin versus syntometrine in the management of the third stage of labour. BJOG 113:1459–1464. doi:10.1111/j.1471-0528. 2006.01105.x
-
Bose P, Regan F, Paterson-Brown S (2006) Improving the accuracy of estimated blood loss at obstetric haemorrhage using clinical reconstructions. BJOG 113:919–924. doi:10.1111/j.1471- 0528.2006.01018.x
